Available At
View Location
We provide diagnostic and therapeutic endoscopy services with wide spectrum.
A protrusion of mucosa and submucosa through the muscular layers of the bowel wall. It has no muscular covering. Because diverticula do not involve all layers of the bowel wall, they are really "false" diverticula. Diverticulum formation may be related either to weakness of the bowel wall at the sites of vessel perforation or to increased intraluminal pressure caused by low dietary fiber and constipation.
Diverticulosis is colonic diverticula without associated inflammation.Diverticulitis is inflammation and infection. Only 15% of patients with diverticulosis develop diverticulitis.
Pain apparently results from perforation of the diverticulum The resulting leakage may be scant and contained within pericolic fat or extensive, involving the mesentery, other organs, or the peritoneal cavity. Sigmoid diverticulitis typically causes pain in the left lower quadrant.

95% of all diverticula occur in the left colon, primarily in the sigmoid colon. Diverticula, however, may occur anywhere in the colon. In Asia, right colonic diverticula are also common.
The sixth or seventh decade of life. Patients younger than 50 with diverticulitis tend to have more complications. Younger patients are more likely than older patients to have right colonic diverticulitis.
A diet high in fiber. Large bulk in the colon decreases segmentation and intraluminal pressure.
Computed tomography (CT) scan, which can also diagnose local complications of diverticulitis.
Yes. Diverticulosis (not-itis) is a common cause of lower gastrointestinal bleeding. Bleeding from diverticulitis is uncommon.
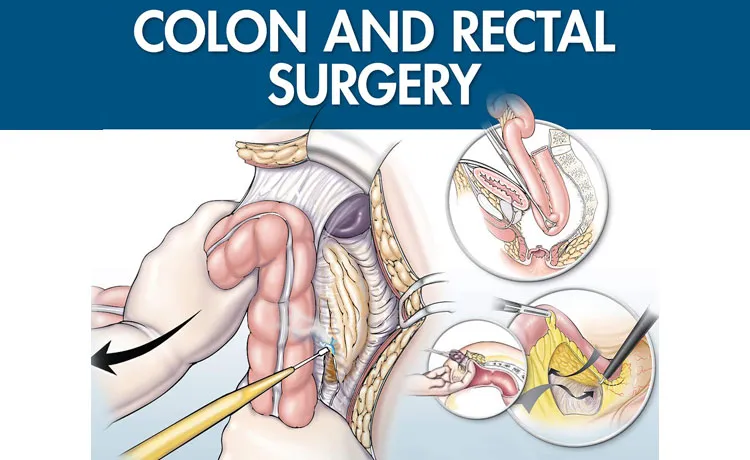
A staged procedure was the standard until recently. Now most patients can be treated with a single procedure that includes sigmoid resection, colonic anastomosis, and primary repair of bladder defect with absorbable suture. A Foley catheter is usually left in place for 10 days after surgery. Some viable tissue should be placed between the colonic and bladder repairs to prevent a recurrent fistula.
Lung, breast or prostate, and colon cancer.
List offew of the presenting symptoms of patients with colorectal cancer. Intermittent rectal bleeding, vague abdominal pain, fatigue secondary to anemia, change in bowel habits, constipation, tenesmus, and perineal pain.
Basic investigation to evaluate a patient with above symptoms.
To evaluate the entire colon and rectum, one may perform stool foe occult blood and proctoscopy/ a colonoscopy. Colonoscopy is most sensitiveand can detect lesions < 1 cm.
List of most common five risk factors for colorectal cancer.
Prior adenomatous polyps, family history of colorectal cancer, age older than 40 years, chronic ulcerative colitis, Crohn's colitis, history of colon cancer, exposure to pelvic radiation for prostate or cervical cancer, and familial polyposis. Hamartomatous polyps (Peutz-Jeghers syndrome), inflammatory polyps, and hyperplastic polyps are not considered premalignant.
Treatment options for colorectal cancer are dependent on the tumor location.
Colonic cancers are more commonly treated with surgical therapy first followed by depends on final biopsy results adjuvant chemotherapy is required
Rectal cancer is now more commonly managed with neo adjuvant therapy followed by surgical therapy.
Which patients with colorectal cancer require adjuvant (postoperative) therapy?
Patients with lymph node involvement should receive chemotherapy postoperatively to treat micrometastases. Two large studies have documented a survival advantage for these patients.
Patients with rectal cancer with a significant chance of local recurrence should be treated with radiation therapy. This may be given preoperatively, postoperatively, or with a combined "sandwich" technique.